Disclaimer:
The information provided in this article is for educational and informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Cardiomyopathy and other heart conditions are complex and require evaluation by a qualified healthcare professional. If you experience symptoms such as shortness of breath, chest pain, palpitations, dizziness, or swelling, you should seek immediate medical attention. Always consult your doctor or a licensed cardiologist before making any decisions related to your health. The authors and publishers of this content do not assume any liability for health-related decisions or outcomes based on the information provided.
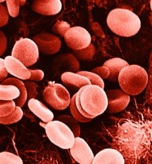
Cardiomyopathy is a complex and potentially life-threatening condition that affects the heart muscle, impairing its ability to pump blood efficiently. Despite advances in medical technology and diagnostic tools, cardiomyopathy is frequently misdiagnosed. Understanding why misdiagnosis occurs is crucial for both patients and healthcare providers, as early and accurate detection is vital to prevent complications such as heart failure, arrhythmias, or sudden cardiac death.
1. The Complexity and Variability of Symptoms
One of the main reasons cardiomyopathy is often misdiagnosed is the wide variability of its symptoms. Patients may present with fatigue, shortness of breath, swelling in the legs, palpitations, dizziness, or chest discomfort. These symptoms overlap with more common conditions such as:
- Asthma or chronic obstructive pulmonary disease (COPD)
- Anemia
- Anxiety or panic disorders
- Obesity-related heart strain
- Coronary artery disease
Because these symptoms are nonspecific, physicians may initially attribute them to other, more common ailments, delaying a correct cardiomyopathy diagnosis.
2. Different Types of Cardiomyopathy Confuse Diagnosis
Cardiomyopathy is not a single disease but a group of disorders, each affecting the heart differently. The main types include:
- Dilated Cardiomyopathy (DCM): Characterized by enlarged, weakened ventricles. Often mistaken for heart failure or chronic fatigue syndrome.
- Hypertrophic Cardiomyopathy (HCM): Thickened heart walls may mimic high blood pressure-related cardiac changes or even be asymptomatic, leading to missed diagnosis.
- Restrictive Cardiomyopathy (RCM): Stiff ventricles restrict blood flow, often confused with constrictive pericarditis or aging-related cardiac stiffness.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): Causes arrhythmias that can be mistaken for benign palpitations or electrolyte imbalances.
The overlap in clinical presentation between types, and with other cardiovascular diseases, makes accurate diagnosis challenging.
3. Limited Awareness Among Patients and Clinicians
Another factor contributing to misdiagnosis is limited awareness. Cardiomyopathy is relatively rare compared to other cardiovascular diseases. Patients may not report subtle symptoms, assuming they are normal or stress-related. Meanwhile, some healthcare providers may not immediately suspect cardiomyopathy, especially in younger patients or those without a family history. This is particularly true for genetic forms of cardiomyopathy, which can be silent for years.
4. Subtle Early Signs and Asymptomatic Progression
Many forms of cardiomyopathy progress silently. Hypertrophic cardiomyopathy, for instance, may not produce noticeable symptoms until a life-threatening event, such as sudden cardiac arrest, occurs. Dilated cardiomyopathy may initially present with mild fatigue or reduced exercise tolerance, which are often overlooked or attributed to lifestyle factors.
Because early signs can be subtle, routine physical exams and basic tests like ECGs may not detect the condition. More advanced imaging, such as echocardiography or cardiac MRI, may be required but are not always performed initially.
5. Overlapping Conditions and Comorbidities
Cardiomyopathy rarely occurs in isolation. Patients often have other cardiovascular risk factors, such as hypertension, diabetes, or coronary artery disease, which can mask the true underlying problem. For example, heart enlargement due to hypertension may be mistaken for dilated cardiomyopathy, or fluid retention from kidney disease may obscure early heart failure symptoms.
6. Diagnostic Limitations
Even with modern diagnostics, cardiomyopathy can be difficult to detect:
- Echocardiograms may not always reveal early structural abnormalities.
- Electrocardiograms (ECG) can appear normal in asymptomatic or early-stage cases.
- Genetic testing is expensive and not routinely done, despite its value in identifying familial forms of the disease.
As a result, patients may undergo repeated misdiagnoses or unnecessary treatments before the correct diagnosis is made.
7. Importance of Family History and Genetic Factors
Many cardiomyopathies, especially hypertrophic and dilated types, have a genetic component. If family history is not thoroughly investigated, clinicians may miss critical clues. A lack of awareness about genetic predisposition leads to delayed recognition, particularly in young adults who might otherwise appear healthy.
8. How Misdiagnosis Impacts Patients
Misdiagnosis or delayed diagnosis can have serious consequences:
- Increased risk of heart failure and hospitalization
- Greater likelihood of life-threatening arrhythmias
- Reduced quality of life due to untreated symptoms
- Emotional and psychological stress from repeated medical visits and uncertainty
9. Strategies to Improve Diagnosis
To reduce misdiagnosis, healthcare providers should:
- Take a comprehensive patient history, including family history of heart disease or sudden cardiac death.
- Use advanced imaging techniques early when cardiomyopathy is suspected.
- Consider genetic counseling and testing for patients with a family history.
- Maintain awareness of subtle or atypical symptoms, particularly in young or seemingly healthy individuals.
- Encourage patients to report all symptoms, even mild ones like fatigue or palpitations.
Conclusion
Cardiomyopathy is often misdiagnosed due to its variable symptoms, overlapping conditions, genetic factors, and subtle early signs. Increasing awareness among both patients and healthcare professionals, combined with the use of advanced diagnostic tools and careful family history assessment, is crucial for timely and accurate detection. Early diagnosis can save lives, improve quality of life, and allow patients to manage the condition more effectively.